Consult your doctor before using Diclofenac, especially if you have a history of heart, liver, or kidney problems, or stomach ulcers.
Understanding Diclofenac
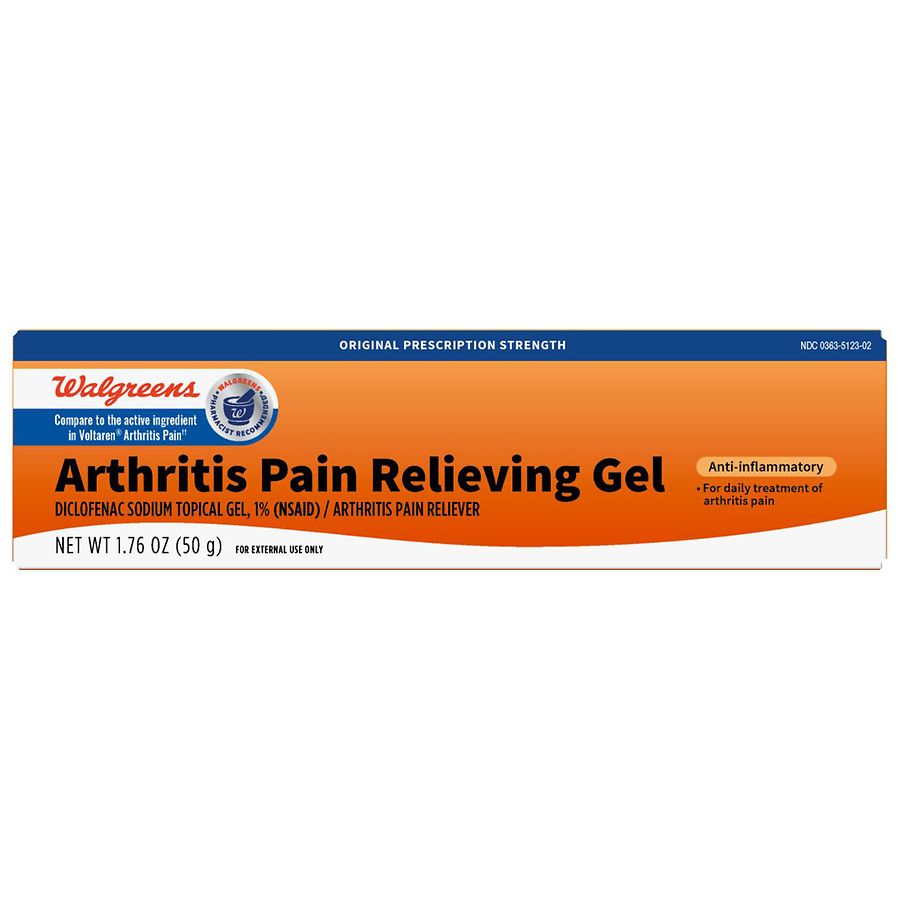
Diclofenac is a nonsteroidal anti-inflammatory drug (NSAID) that reduces pain and inflammation. It’s available in various forms: tablets, capsules, topical gels, and injections. The choice depends on your condition and doctor’s recommendation. Oral forms generally treat widespread pain, while topical gels target localized pain like muscle aches.
Dosage and Administration
Your doctor determines the correct dosage based on your specific needs and health status. Never exceed the recommended dose. Follow instructions carefully regarding frequency and timing of administration. For example, some formulations are best taken with food to reduce stomach irritation.
Potential Side Effects
- Gastrointestinal Issues: Stomach pain, nausea, heartburn, and ulcers are possible. Taking Diclofenac with food can often mitigate these.
- Cardiovascular Effects: Increased risk of heart attack or stroke. This risk is higher with prolonged use and higher doses.
- Kidney Problems: Diclofenac can affect kidney function, especially in those with pre-existing conditions. Regular monitoring may be necessary.
- Liver Issues: Rare, but liver damage is a potential side effect. Report any unusual symptoms immediately.
Interactions with Other Medications
Diclofenac can interact negatively with certain medications, including anticoagulants (blood thinners), diuretics, and other NSAIDs. Always inform your doctor of all medications, supplements, and herbal remedies you are currently taking.
Precautions and Warnings
Avoid alcohol while using Diclofenac as it increases the risk of gastrointestinal bleeding. If you experience any severe side effects, such as chest pain, shortness of breath, or severe stomach pain, seek immediate medical attention. Pregnancy and breastfeeding require careful consideration; discuss with your doctor before using Diclofenac.
Alternatives to Diclofenac
If Diclofenac is unsuitable, your doctor can explore other pain and inflammation management options, such as other NSAIDs, paracetamol, or other treatments depending on the specific condition.
Monitoring and Follow-up
Regular check-ups with your doctor are vital, particularly for those taking Diclofenac long-term. This allows for monitoring of potential side effects and adjustments to treatment as needed.
Interactions with Other Medications and Substances
Always inform your doctor or pharmacist of all medications you are taking, including over-the-counter drugs, herbal remedies, and supplements, before starting diclofenac. This includes prescription drugs, such as anticoagulants (blood thinners like warfarin), lithium, methotrexate, and certain diuretics. These medications can interact with diclofenac, potentially increasing the risk of bleeding, kidney problems, or other adverse effects.
Specific Interactions
Combining diclofenac with nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen increases the risk of stomach ulcers and bleeding. Concomitant use with potassium-sparing diuretics can lead to elevated potassium levels in the blood (hyperkalemia). Alcohol consumption while taking diclofenac raises the chance of gastrointestinal complications. Cyclosporine and tacrolimus interactions can impair kidney function. Careful monitoring is advised when combining diclofenac with selective serotonin reuptake inhibitors (SSRIs) or other antidepressants due to the increased risk of bleeding. Finally, be aware that diclofenac might reduce the effectiveness of certain antihypertensive medications.
Your doctor can help you manage these potential interactions by adjusting dosages or suggesting alternative treatments. Never stop or change your medications without consulting your doctor first. Open communication is key to safe and effective medication management.