Yes, Lasix (furosemide) is a potent diuretic that frequently lowers blood pressure. It achieves this by increasing the excretion of sodium and water from your body, reducing blood volume and subsequently, blood pressure.
However, the extent of blood pressure reduction varies significantly depending on individual factors. Your doctor will consider your specific health status, including other medications you take and pre-existing conditions, when determining the appropriate dosage and monitoring its effects. Regular blood pressure checks are crucial while on Lasix.
Important Note: Lasix is a prescription medication. Never start or stop taking it without consulting your physician. Self-medicating can be dangerous. They will assess your needs and monitor you for potential side effects, such as dehydration and electrolyte imbalances. These are serious concerns that need professional medical management.
Remember: This information is for educational purposes only and should not be considered medical advice. Always consult with a healthcare professional for personalized guidance regarding your health and medication.
- Does Lasix Drop Blood Pressure?
- How Lasix Works to Reduce Fluid Volume
- The Result: Increased Urine Production
- Potassium Considerations
- Lasix’s Direct Impact on Blood Pressure: A Closer Look
- Mechanism of Action
- Individual Variability
- Factors Influencing Blood Pressure Reduction with Lasix
- Potential Side Effects Related to Blood Pressure Changes
- Dehydration and Electrolyte Imbalances
- Orthostatic Hypotension
- Other Potential Side Effects
- When to Seek Medical Attention
- Disclaimer
- Lasix and Other Blood Pressure Medications: Interactions
- When to Consult a Doctor About Lasix and Blood Pressure
Does Lasix Drop Blood Pressure?
Yes, Lasix (furosemide) can lower blood pressure. It’s a potent diuretic, meaning it increases urine production by flushing excess sodium and water from your body. This reduced blood volume directly lowers blood pressure.
However, the extent of blood pressure reduction varies significantly depending on factors like your individual physiology, the dose of Lasix prescribed, and other medications you’re taking. Some individuals experience a dramatic drop, while others see a more modest decrease.
Always consult your doctor before starting or altering Lasix dosage. They will carefully monitor your blood pressure and adjust the medication as needed to achieve the desired effect without causing harmful side effects. Regular blood pressure checks are vital when taking Lasix.
Potential side effects of Lasix include dehydration, dizziness, and electrolyte imbalances. These are often manageable with proper hydration and medical supervision. Report any concerning symptoms to your physician immediately.
Lasix is not a first-line treatment for hypertension in most cases. Your doctor will likely prescribe it alongside other blood pressure medications or only in specific situations like managing fluid overload associated with heart failure or kidney disease.
Remember, this information is for educational purposes and does not substitute professional medical advice. Always discuss your treatment plan with your doctor to ensure safe and effective management of your blood pressure.
How Lasix Works to Reduce Fluid Volume
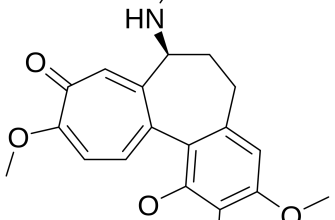
Lasix, or furosemide, acts as a powerful diuretic by directly targeting your kidneys. It inhibits the sodium-potassium-chloride co-transporter (NKCC2) in the thick ascending limb of the loop of Henle. This specific mechanism prevents the reabsorption of sodium, chloride, and potassium back into your bloodstream.
The Result: Increased Urine Production
By blocking reabsorption, Lasix forces your kidneys to excrete a larger volume of these electrolytes along with water. This leads to a significant increase in urine production, effectively reducing excess fluid buildup in your body. This reduction in fluid volume is what directly contributes to lower blood pressure.
Potassium Considerations
Because Lasix impacts potassium reabsorption, regular blood tests monitoring potassium levels are vital to prevent imbalances. Your doctor will adjust your dosage or prescribe potassium supplements if necessary, ensuring your potassium levels remain within the safe range.
Lasix’s Direct Impact on Blood Pressure: A Closer Look
Lasix, or furosemide, directly lowers blood pressure by increasing urine production. This diuretic action reduces blood volume, thus decreasing the pressure exerted on artery walls. The effect is usually noticeable within a few hours of administration. Dosage significantly influences the magnitude of blood pressure reduction; higher doses generally lead to greater decreases.
Mechanism of Action
Lasix inhibits sodium and chloride reabsorption in the loop of Henle, a key part of the kidney’s filtration system. This inhibition forces the kidneys to excrete more sodium and water, leading to a decrease in extracellular fluid volume and subsequently, blood pressure. This process also affects potassium levels, potentially leading to hypokalemia, a condition requiring monitoring.
Individual Variability
The extent to which Lasix lowers blood pressure varies among individuals. Factors such as age, kidney function, and overall health status influence the response. Patients with pre-existing conditions like dehydration or heart failure may experience more pronounced effects. Regular monitoring of blood pressure and electrolyte levels is crucial.
Factors Influencing Blood Pressure Reduction with Lasix
Lasix’s effectiveness in lowering blood pressure depends on several interacting elements. Understanding these factors helps optimize treatment.
| Factor | Influence on Blood Pressure Reduction | Practical Implications |
|---|---|---|
| Dosage | Higher doses generally lead to greater diuresis and subsequent blood pressure reduction, but increased risk of side effects. | Doctors carefully adjust dosage based on individual response and health status. |
| Hydration Status | Dehydration diminishes Lasix’s effectiveness. Adequate fluid intake is vital. | Patients should maintain proper hydration levels by drinking sufficient water. |
| Underlying Health Conditions | Conditions like heart failure or kidney disease impact fluid retention and Lasix’s efficacy. | Treatment requires individualized consideration of underlying health issues. |
| Concomitant Medications | Certain medications may interact with Lasix, affecting its blood pressure-lowering effects. | Patients should provide a full list of medications to their physician. |
| Diet | A high-sodium diet can counteract Lasix’s diuretic effect. Reducing sodium intake boosts results. | Dietary modifications, including sodium restriction, are important for optimal outcomes. |
| Individual Response | People respond differently to Lasix; some experience significant blood pressure drops, while others have a less dramatic response. | Regular monitoring of blood pressure is necessary to personalize treatment. |
Regular blood pressure checks and open communication with your healthcare provider are key for managing your blood pressure effectively while taking Lasix.
Potential Side Effects Related to Blood Pressure Changes
Lasix, while effective in lowering blood pressure, can cause side effects related to this pressure drop. Understanding these is key to safe usage.
Dehydration and Electrolyte Imbalances
Lasix is a diuretic, meaning it increases urination. This can lead to dehydration if you don’t drink enough fluids. Dehydration, in turn, can worsen dizziness and lightheadedness. Electrolyte imbalances, such as low potassium (hypokalemia), sodium (hyponatremia), or magnesium, are also possible. These imbalances can manifest as muscle weakness, cramps, irregular heartbeat, or even more serious complications.
- Recommendation: Drink plenty of water and consider electrolyte-rich drinks as directed by your doctor.
- Monitoring: Regular blood tests can check for electrolyte imbalances.
Orthostatic Hypotension
A sudden drop in blood pressure upon standing can cause dizziness or fainting (orthostatic hypotension). This is more likely if you’re already dehydrated or on other blood pressure medications.
- Recommendation: Rise slowly from a lying or sitting position. Avoid sudden movements.
- Prevention: Maintain adequate hydration and inform your doctor about all medications you are taking.
Other Potential Side Effects
Other side effects, unrelated to blood pressure changes, include but are not limited to:
- Increased thirst
- Frequent urination
- Drowsiness
- Headache
- Nausea or vomiting
- Dizziness
When to Seek Medical Attention
Contact your doctor immediately if you experience severe dizziness, fainting, rapid heartbeat, or significant muscle weakness. These may indicate a serious complication requiring immediate medical intervention.
Disclaimer
This information is for educational purposes only and does not replace professional medical advice. Always consult your doctor before starting or changing any medication.
Lasix and Other Blood Pressure Medications: Interactions
Always inform your doctor about all medications you’re taking, including over-the-counter drugs and supplements, before starting Lasix. This is crucial for preventing dangerous interactions.
Lasix, a diuretic, can interact significantly with several blood pressure medications. These interactions can either boost or lessen the effectiveness of both Lasix and your other medications, potentially leading to either dangerously low blood pressure or insufficient blood pressure control.
- ACE inhibitors (e.g., lisinopril, ramipril): Combining Lasix with ACE inhibitors can increase the risk of low blood pressure and kidney problems. Your doctor will carefully monitor your potassium levels and blood pressure.
- Angiotensin II receptor blockers (ARBs) (e.g., valsartan, losartan): Similar to ACE inhibitors, ARBs combined with Lasix raise the risk of low blood pressure and kidney complications. Close monitoring is necessary.
- Beta-blockers (e.g., metoprolol, atenolol): While not as directly interacting as ACE inhibitors or ARBs, concurrent use with Lasix may require dosage adjustments to avoid excessively low blood pressure. Regular blood pressure checks are vital.
- Potassium-sparing diuretics (e.g., spironolactone, amiloride): Combining Lasix with these diuretics can lead to dangerously high potassium levels (hyperkalemia). Your doctor will regularly test your potassium levels.
- NSAIDs (e.g., ibuprofen, naproxen): Nonsteroidal anti-inflammatory drugs can reduce the effectiveness of Lasix, potentially hindering blood pressure control. Your doctor might adjust your Lasix dosage or recommend alternative pain relievers.
This list isn’t exhaustive; other medications may also interact. Always consult your physician or pharmacist before mixing medications. They can help determine the safest approach for your individual needs and monitor your progress.
- Regular monitoring: Your doctor will likely schedule frequent check-ups to monitor your blood pressure and electrolyte levels (potassium, sodium).
- Dosage adjustments: Based on your response to the medication, your doctor might adjust the dosages of Lasix or other medications to optimize treatment.
- Open communication: Report any new symptoms or side effects to your doctor immediately.
When to Consult a Doctor About Lasix and Blood Pressure
Experience a sudden, significant drop in blood pressure, dizziness, or lightheadedness after taking Lasix? Contact your doctor immediately. These could be signs of dangerously low blood pressure (hypotension).
Notice persistent thirst, dry mouth, or decreased urination despite taking Lasix? These could indicate dehydration, a serious side effect. Schedule an appointment with your doctor to discuss your symptoms and adjust your medication or fluid intake.
Your blood pressure readings remain consistently high even while taking Lasix? Your doctor needs to reassess your treatment plan. Regular monitoring and potential adjustments are crucial for effective blood pressure management.
Develop muscle weakness, cramps, or irregular heartbeat? These are potential side effects warranting immediate medical attention. Inform your doctor about these symptoms without delay.
Experience any new or worsening symptoms, even seemingly unrelated to Lasix, after starting the medication? Consult your doctor to rule out medication interactions or other health issues.
Before starting or adjusting Lasix, always discuss your health status and other medications with your physician. This ensures safe and effective management of your condition.